Is Long COVID Real?
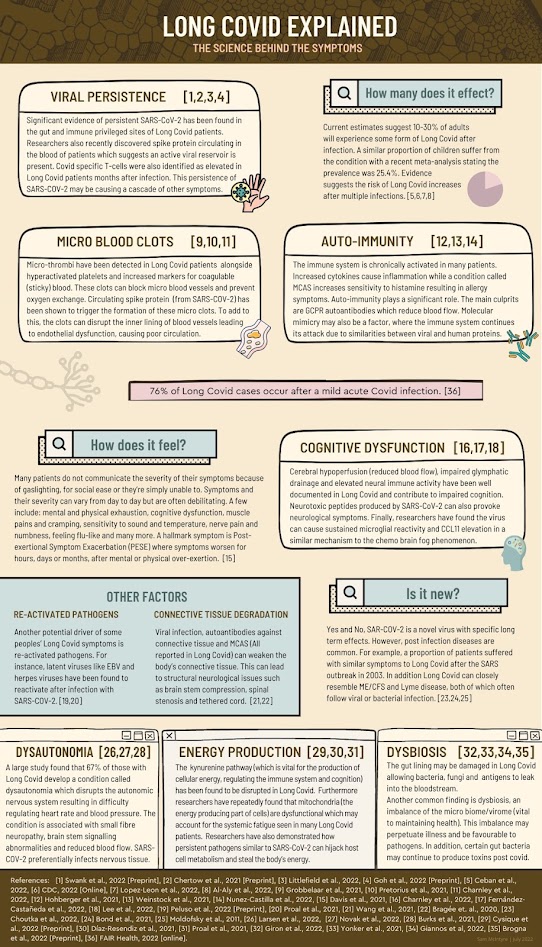
Long COVID continues to debilitate a significant number of U.S. adults — 7.5%, or 1 in 13,1 are struggling with a range of symptoms that make up this complex condition. Among those who have had COVID-19, 11% say they currently have long COVID,2 which often includes unrelenting fatigue, respiratory symptoms, neurological difficulties and joint or muscle pain, all of which may become worse after physical or mental exertion.3
Long COVID symptoms share many similarities with post-jab injuries, and it's likely both are rooted in mitochondrial dysfunction. Now, however, there's a growing trend to label long COVID and injuries from COVID-19 shots "functional neurological disorders" (FND), making some patients feel like the medical community thinks their symptoms are "all in their head."
Is Long COVID Akin to 'Hysteria'?
In an article for TNR, journalist Natalie Shure writes, "The most direct precursor to FND is something you've probably heard of: hysteria."4 For centuries, women were diagnosed with "hysteria" to describe a mental disorder that could give rise to physical and other symptoms ranging from seizures and anxiety to pain and paralysis.
It was, in short, a catch-all diagnosis used to categorize symptoms that weren't otherwise understood or solvable using the mainstream medical treatments of the time. Eventually, much controversy and research suggested it was the hysteria diagnosis that was the delusion.
The medical community was then left to go back where it started from — a range of troubling symptoms, such as myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), with no obvious solution still existed. "In the 1990s and early 2000s, it was becoming clear that illnesses previously known as hysteria hadn't simply vanished," Shure wrote:5
"[Researchers, including neuropsychiatrist Alan Carson,] began to study the symptoms with a neurological lens, conceiving of them as misfiring brain signals rather than a Freudian cry for help.Rebranding hysteria as FND was to reject the notion that the best way to understand functional paralysis was as a subconscious repression of childhood memories. Rather, it was an interruption in the brain processing that facilitates the executive function of your legs — a blip that could be triggered by all sorts of things."
It's now being suggested that "some post-COVID symptoms may be produced by the brain," Shure notes. "Does that make them any less real?" For instance, half of people with long COVID symptoms fit the criteria to be diagnosed with ME/CFS and some in the community have suggested the symptoms could be due to ME/CFS, which often flares up after viral infection.6
But it's far from that simple, as symptoms of long COVID include everything from shortness of breath and pounding heart to dizziness, brain fog and depression. Even the CDC states:7
"People with post-COVID conditions may develop or continue to have symptoms that are hard to explain and manage. Clinical evaluations and results of routine blood tests, chest x-rays, and electrocardiograms may be normal.The symptoms are similar to those reported by people with ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome) and other poorly understood chronic illnesses that may occur after other infections. People with these unexplained symptoms may be misunderstood by their healthcare providers, which can result in a long time for them to get a diagnosis and receive appropriate care or treatment."
Can FND Explain Long COVID?
Shure cites several examples of individuals recovering from long COVID using "a biopsychosocial framework." This includes Paul Garner, professor at the Liverpool School of Tropical Medicine, who says he recovered from severe long COVID symptoms using techniques from those in the ME/CFS community:8
"I learnt that our primitive and unconscious defense mechanisms against injury and infection in the brain and other parts of the body sometimes get disturbed, giving false fatigue alarms. A vicious cycle is set up, of dysfunctional autonomic responses being stimulated by our subconscious. These neural tracks become established like tire tracks in mud.I learnt that I could change the symptoms I was experiencing with my brain, by retraining the bodily reactions with my conscious thoughts, feelings, and behavior. Over the following weeks, with support, I learnt how to do this. I suddenly believed I would recover completely.
… I write this to my fellow covid-19 long haulers whose tissues have healed. I have recovered. I did this by listening to people that have recovered from CFS/ME, not people that are still unwell; and by understanding that our unconscious normal thoughts and feelings influence the symptoms we experience."
Still, there's a lack of consensus and definitions when it comes to FND and its potential treatments, even among those who are considered experts in the field. Meanwhile, since stress is also a key component in FND, it's possible long COVID could be triggered by pandemic trauma along with the viral infection. According to Shure:9
"In other words, stress could exacerbate FND, and someone with FND could overfocus on symptoms and essentially turn up their volume, requiring brain processing for actions that should be automatic. As Carson put it to me, the term 'functional neurological disorder' should be reserved for neurological symptoms like weakness, seizures, memory loss, or cognitive issues.'Functional symptoms' and 'functional disorders' are largely used interchangeably about other parts of the body. Irritable bowel syndrome, for example, is widely theorized to be a functional disorder.
Meanwhile, conditions like depression and anxiety frequently include symptoms most people would describe as physical. It's even possible to have functional and nonfunctional symptoms at the same time. 'We wonder why people get confused!' Carson quipped."
There are also many additional theories as to what may be causing long COVID, many of them rooted in biological causes. Research presented by Dr. Bruce Patterson at the International COVID Summit in Rome, in September 2021, for instance, suggests monocytes, shown to cause lung damage in patients with acute COVID, are involved in long COVID.10,11
Another theory, put forth by Harald Prüss, a neurologist at the German Center for Neurodegenerative Diseases and the Charité University Hospital in Berlin, suggests antibodies targeting the SARS-CoV-2 spike protein might be causing the damage.12
Many Experience Post-Jab Long COVID
It's interesting to note that, in one study from early in the pandemic, more than two-thirds of those reporting long COVID symptoms had negative antibody tests, suggesting at least some of them didn't even have COVID-19.13 Meanwhile, many COVID jab recipients report long COVID-like symptoms.
As reported by Science magazine, "In rare cases, coronavirus vaccines may cause long COVID-like symptoms,"14 which can include (but is not limited to) brain fog, memory problems, headaches, blurred vision, loss of smell, nerve pain, heart rate fluctuations, dramatic blood pressure swings and muscle weakness. The feeling of "internal electric shocks" are also reported.
The primary difference15 between post-jab long COVID and long COVID symptoms after infection is that in people who get it from the infection, early treatment was withheld and the resulting infection severe. Post-jab long COVID, on the other hand, can occur either after very mild breakthrough infection or no breakthrough infection at all.
The Dark Side of FND for COVID Jab Injuries
With many of the symptoms of COVID shot injuries mirroring those of long COVID, we're now also seeing the use of FND as a diagnosis to explain away adverse reactions to COVID-19 shots.
One case involves Maddie de Garay, who was a healthy 12-year-old when she signed up for Pfizer's COVID-19 trial for 12- to 15-year-olds. She suffered a severe systemic adverse reaction to her second dose of the shot, however, and struggled through 11 ER visits and four hospital admissions in the year and a half that followed.
Injuries from the shot have left her unable to walk or eat — she receives her nutrition via a feeding tube — and suffering from constant pain, vision problems, tinnitus, allergic reactions and lack of neck control.16
As though the physical trauma wasn't enough, Maddie and her family were continually dismissed by the medical professionals put in place to help, ignored by the U.S. Food and Drug Administration and denied the care needed to help Maddie.
In Pfizer's April 2021 disclosure of Maddie's case to the FDA, it's stated only that she had "functional abdominal pain."17 Then, a day before Pfizer submitted their request for emergency approval of the COVID-19 shot for 12- to 15-year-olds to the FDA, they added functional neurological disorder as a diagnosis in Maddie's chart,18 blaming the side effects from the shot on FND.
Further, once this assessment was made, her physician, Dr. Amal Assa'ad at Cincinnati Children's Hospital, went so far as to advise against any further investigation, even though Maddie was a participant in a clinical trial:19
"My assessment is that Madeline has a functional impairment that is not organic in nature … I also discourage further work up since this is usually detrimental in functional disorders because it drives the patient to thinking that there must be something wrong that is indicating all this work up. It also delays the necessary psychologic intervention that is needed to help resolve the functional disorder."Help for Long COVID and Post-Jab Symptoms
The Front Line COVID-19 Critical Care Working Group's (FLCCC) I-RECOVER20 protocol can be downloaded in full,21 giving you step-by-step instructions on how to treat long COVID22 and/or reactions from COVID-19 injections.23 I also recently summarized strategies to optimize mitochondrial health if you're suffering from long COVID, with a focus on boosting mitochondrial health.
For starters, to allow your body to heal you'll want to minimize EMF exposure as much as possible. Your diet also matters, as the cristae of the inner membrane of the mitochondria contains a fat called cardiolipin, the function of which is dependent on the type of fat you get from your diet.
The type of dietary fat that promotes healthy cardiolipin is omega-3 fat, and the type that destroys it is omega-6, especially linoleic acid (LA), which is highly susceptible to oxidation. So, to optimize your mitochondrial function, you want to avoid LA as much as possible, and increase your intake of omega-3s.
Primary sources of LA include seed oils used in cooking, processed foods and restaurant foods made with seed oils, condiments, seeds and nuts, most olive oils and avocado oils (due to the high prevalence of adulteration with cheaper seed oils), and animal foods raised on grains such as conventional chicken and pork.
Another major culprit that destroys mitochondrial function is excess iron — and almost everyone has too much iron. Copper is also important for energy metabolism, detoxification and mitochondrial function, and copper deficiency is common. Other strategies include sun exposure and near-infrared light therapy, time-restricted eating, NAD+ optimizers and methylene blue, which can be a valuable rescue remedy.
Whether long COVID has a functional element to it or not, each individual suffering deserves access to the full range of potential treatments. Unfortunately, this often isn't the case, especially if symptoms are dismissed as purely psychological in nature. If you improve your mitochondrial function and restore the energy supply to your cells, you'll significantly increase your odds of reversing the problems caused by the jab or the virus.
- 1 U.S. CDC, National Center for Health Statistics June 22, 2022
- 2 KFF January 26, 2023
- 3, 7 U.S. CDC, Long COVID or Post-COVID Conditions December 16, 2022
- 4, 5, 6, 9, 13 TNR December 8, 2022
- 8 thebmjopinion January 25, 2021
- 10 Frontiers in Immunology January 10, 2022 DOI: 10.3389/fimmu.2021.746021
- 11 Health Rising July 21, 2021
- 12, 14 Science January 20, 2022
- 15 Washington University School of Medicine May 25, 2022
- 16, 18 Life Funder, Help Maddie de Garay get essential medical care
- 17 The Highwire, Rigged: Maddie’s Story August 13, 2022, 1:04
- 19 The Highwire, Rigged: Maddie’s Story August 13, 2022, 21:03
- 20, 21 FLCCC Alliance, I-RECOVER
- 22 FLCCC Alliance, I-RECOVER, Long COVID
- 23 FLCCC Alliance, I-RECOVER, Post-Vaccine Treatment Protocol

.png)



.png)
.png)



Comments